What is it?
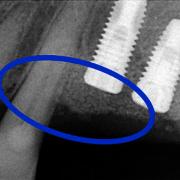
There are some anatomical conditions of the jaw and the jaw bones that do not allow insertion of an implant with a diameter and length sufficient enough to ensure the long-term stability of the prosthesis.
This occurs especially in patients who have been edentulous (without teeth) for a long period of time, but it may be necessary to resort to regenerative therapy even after traumatic tooth extractions or major infections of the alveolar bone.
The loss of teeth, even the loss of a single dental element, causes bone loss in response to the absence of the bio-mechanical stimuli of mastication. In other words, the bone is no longer demanded by the force transmitted from the roots of the teeth and goes into atrophy.
At the basis of regeneration is the formation and stability of blood clots and the fibrin network contained in the area of the defect, resulting in differentiation of the undifferentiated mesenchymal cells from blood in osteoblasts, osteocytes, osteoclasts or in the cells of the bone. From the beginning, these cells produce new bone tissue thanks to its lamellar structure and the formation of "osteon."
When, for anatomical reasons, it is not possible to obtain stability of the blood clot and, therefore, bone generation, we must resort to surgical techniques and bio-materials (bone grafts) that provide the “scaffolding” for the clot and thus allow it to mature into bone.
How can bone loss be rectified?
The different kinds of bone grafts are categorised as:
- Autologous: taken from the same patient.
- Homologous: taken from a donor.
- Heterologous: taken from a different species.
- Synthetic (alloplastic): created in a laboratory.
The bio-materials that are not autologous are sterilised, subjected to viral inactivation and hygenicized before they are released to the market, offering a biologically safe option that is devoid of any health risk.
All bio-materials that we use are also equipped with a card that certifies safety traceability, in addition to 10-year scientific followup evaluations to ensure their effectiveness.
How does regeneration work?
The bone graft represents the scaffold for the process of regeneration. It is used for the migration and proliferation of undifferentiated cells from the blood through proteins in the membrane; these proteins bind to the “skeleton” of the cell in the extracellular matrix playing an important role, along with the growth factors, for cell migration and differentiation. Basically, the cells will “climb” on this scaffold where they will find the proper stability to support them as they mature.
Then, after a certain period of time in contact with the biological environment, the scaffold undergoes changes that lead to the partial or complete substitution of the patient’s mature bone.
There are different surgical techniques, each with its own particular indications, that enable complete regeneration in the area of the bone defect.
Today, we have a wide variety of bone substitutes (bio-materials) that can help repair the loss of significant quantities of intra-oral bone, resulting in greater post-operative comfort for the patient.
Depending on the type of bone defect, in order to ensure the stability of the bio-material inserted, resorbable collagen membranes or non-resorbable, titanium-reinforced membranes (which must eventually be removed for regeneration to occur) may be implemented. The particles of bio-material are then protected within the oral cavity by a ‘tent’ that covers them entirely.
In other cases, it may be necessary to resort to the use ofbone blocks which are shaped to fit and are then screwed into the area covering the bone defect.
On average, after a period of six months, there is mature bone which is ready to support the insertion of prosthetic implants.